Emergency medicine residency


The Corewell Health – Grand Rapids/Michigan State University Emergency Medicine Residency, follows a PGY 1-3 format, accepting ten residents annually. Residents train at two primary locations, Corewell Health Butterworth Hospital (part of Corewell Health Grand Rapids Hospitals) and Helen DeVos Children’s Hospital. Our curriculum is ever changing to keep pace with the rapid evolution of emergency medicine. We use a variety of teaching methods to help residents learn the foundational knowledge of emergency medicine and hone critical thinking skills. We have a robust interactive academic curriculum and simulation activities help to further develop the procedural skills necessary to practice emergency medicine.
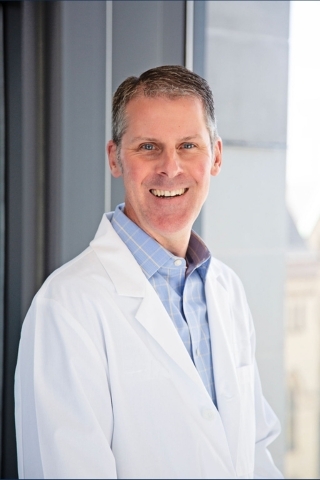
Dr. Jason Seamon: 2020 EMRA Residency Director of the Year
Dr. Seamon has been the program director for Corewell Health – Grand Rapids/Michigan State University Emergency Medicine Residency since 2018. He is one of approximately 270 emergency medicine program directors across the country. Dr. Seamon is the first program director to receive this award from our program and is only the second program director from Michigan to receive this award in its 20-year history.
Despite the residency challenges of the Covid-19 pandemic, Dr. Seamon has remained steadfast in the face of adversity, continued to innovate through virtual education and strengthened our residency through his guidance, transparency and communication. He provides incredible mentorship and consistently empowers his team to take action, to support one another and to be innovative.
From the Program Director
Welcome to the emergency medicine residency at Corewell Health in West Michigan, in partnership with Michigan State University College of Human Medicine! I have been affiliated with this residency program for over thirteen years. I am passionate about academic emergency medicine and am excited to share with you a little about our program.
Corewell Health in West Michigan is a very special hospital and we are a unique residency program. First, we are the seventh oldest EM residency program in the entire country, established in 1977. With over 200 accredited EM residency programs, you will get a true sense of the important place we hold in the history of emergency medicine. Second, we are one of the busiest singles-site ED systems in the entire country, seeing a combined annual volume of over 168,000 patients. We maximize your exposure in the emergency department to take advantage of these clinical opportunities. Third, we are both a Level I Adult Trauma Center and a nationally recognized Children’s Hospital. With us it’s not either/or, it’s both! Finally, we provide a valuable experience that supports your education and wellbeing.
On behalf of our entire residency, I thank you for your interest in emergency medicine and in our program. We look forward to seeing you soon!
Best,
Jason P. Seamon, DO, MHS, FACEP
Program Director, Emergency Medicine Residency
Corewell Health - Grand Rapids/Michigan State University
Watch Dr. Seamon at the Emergency Medicine Residents' Association Hangout
Overview
Program aim
- To produce emergency medicine physicians who are safe, competent and qualified to practice independently
Corewell Health Butterworth Hospital (part of Corewell Health Grand Rapids Hospitals)
- More than 7,600 inpatient admissions annually
- Level 1 Trauma Center
- Low acuity Fast Track covered by physician extenders – allows residents to see more critical cases
- 679 bed hospital, including Fred and Lena Meijer Heart Center
- 20 observation beds/chest pain center
- Certified Stroke Center
- In-department CT and radiology, MRI available 24 hours/day
- Social workers and translators in the department 24 hours/day
Corewell Health Helen DeVos Children's Hospital (part of Corewell Health Grand Rapids Hospitals)
- 20 pediatric beds plus clinical decision unit/observation unit
- Residents provide care in both the acute care and fast track areas of the pediatric emergency department
- Level I Pediatric Trauma Center
- Nearly 200 pediatric physicians in more than 50 pediatric specialties and programs
- In-department CT and radiology, MRI available 24 hours/day
- Social workers and translators in the department 24 hours/day
Education
High volume emergency departments in world-class facilities - Our primary training sites are housed within Corewell Health Butterworth Hospital (part of Corewell Health Grand Rapids Hospitals) and Corewell Health Helen DeVos Children's Hospital (part of Corewell Health Grand Rapids Hospitals). The annual emergency department census exceeds 110,000 patients at Butterworth Hospital and over 50,000 at Helen DeVos Children’s Hospital. Both facilities contain the latest medical technology and state-of-the-art equipment to help provide the best care possible for patients.
Exposure to a wide variety of patients - We are fortunate to interact with patients from all walks of life every day. Patients of all ages and with a wide variety of medical conditions present for evaluation and treatment to both hospitals. You will be well trained in all aspects of emergency medicine care upon completion of our program.
Faculty dedicated to medical education - Our faculty takes your residency training seriously. We have numerous, experienced clinicians/educators who actively engage themselves in helping our residents learn the art and science of emergency medicine.
Dynamic educational curriculum - Our curriculum is ever changing to keep pace with the rapid evolution of emergency medicine. We use a variety of teaching methods to help residents learn the foundational knowledge of emergency medicine and hone critical thinking skills. We utilize low- and high-fidelity simulation activities to help further develop and hone the procedural skills necessary to practice emergency medicine.
Exceptional ultrasound training - The ultrasound training that you will experience is hands-on and top-notch. From ocular to FAST exams, you will be well prepared in the use and interpretation of ultrasound by the time you graduate. Two educators who have expertise in ultrasound oversee ultrasound training. Our residents’ ultrasound education is complimented by an ultrasound fellowship.
Medical toxicology rotation - Few institutions have a dedicated team of physicians and learning rotation devoted to the care of toxicological patients. Your toxicology experience will help you understand the presentation and pathophysiology of a vast array of poisons and how to better care for these types of patients.
Training tomorrow’s leaders in emergency medicine - We have a long and proud tradition of training excellent emergency medicine physicians. Whether you become a community-based clinician, or pursue a career in academics, the learning experiences and skills that you will take away with you will prepare you for your chosen career path. Many of our graduates have attained leadership positions within their communities, institutions, and the house of emergency medicine.
A program that values resident development (personal and professional) and wellness - We invest in the personal and professional development of our residents; each resident is paired with a mentor to help guide them through the challenges that often accompany residency training. Wellness is one element to our program’s success. Bear witness to the smiles on the residents’ faces during your interview day! As an example of our wellness activities, our residents participate in an annual summer retreat on the sandy shores of Lake Michigan, and take to the slopes of northern Michigan for a winter retreat immediately following the in-service training exam.
Didactics
- Quarterly interactive sessions: Ultrasound (PGY-1), Research (PGY-2), EMS/career planning (PGY-3)
- Intensive reading program
- Monthly journal club
- Regular procedure and simulation labs
- Monthly EKG and radiology club
- Monthly morbidity and mortality review
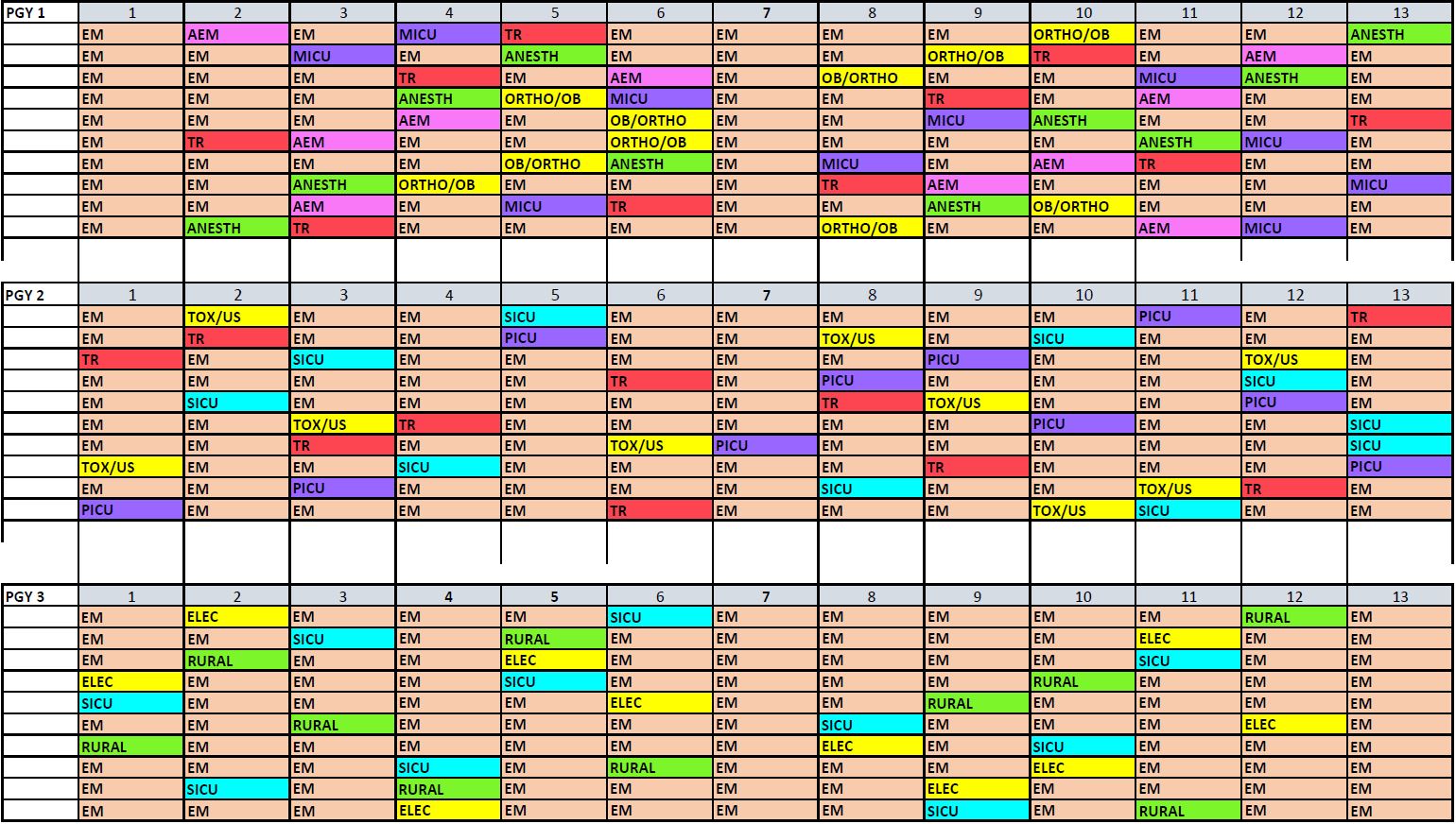
Sample block schedule
Research
Research support is available to you in the level of your interest. We have a specific faculty member dedicated to coordinating and assisting you. Our research department and the Van Andel Institute provide world-class research and support.
During your PGY-2 year, we provide an educational track that exposes you to research and fulfills the program and ACGME requirements. The PGY-2 class gathers one hour each month during our Thursday conference for a “year-specific breakout session”. These sessions serve to provide focused education with regards to research for PGY-2 residents.
Research is the theme of our second year-specific didactic sessions. During monthly class meetings, Dr. Jeff Jones covers various key research elements. The first half of the year focuses on learning the “tools” of research. During this time, each resident puts together an interesting case report along with a faculty mentor. These case reports are presented at a local research meeting each spring. A few reports each year are presented at national conferences. Our core faculty hold an academic appointment at Michigan State University College of Human Medicine and are involved in scholarly activity. Click here to see emergency medicine research highlights.
An original clinical or bench research project is occasionally performed, but always encouraged for those eager research-oriented residents. The emergency medicine department has a strong clinical research program which has been in place for over 25 years with a goal to improve emergency care by creating an environment of inquiry and scholarship. During the past 12 months, faculty, residents and students have presented over 50 different research projects nationally and internationally.
Most residents focus their efforts to learn the skill sets needed for using the biomedical literature to answer clinical questions and hone evidence based medicine critical analysis. These skills are applied in the second half of the year by formulating a clinical question that has not been answered clearly in the medical literature. The best evidence about this question is critically appraised and a brief summary of the analysis is written that often results in a published original review.
For research support, the scholarly activity support team can assist you. The scholarly activity support team also offers biostatistics consultation, and poster preparation. Residents will be expected to submit their work for presentation at an institutional Research Day.
Resident life

Giving back to our community through volunteerism means so much to our program. In June 2019, residents and faculty participated in a Habitat for Humanity project called Plaza Roosevelt. We look forward to doing this every year.
Emergency medicine residents and faculty at the Ballistics Lab at Kent County Conservation League


Emergency medicine residents at a wellness event at Cannonsburg Ski Area.
Emergency medicine residents at Camp Blodgett for the 2023 summer retreat.
.jpg)
Application requirements
- Applications are accepted through the Electronic Residency Application Service only. Application deadline is November 1.
- Include dean’s letter and three letters of recommendation.
We also require a personal statement, medical school transcript and a score from your USMLE Step 1 or COMLEX Step 1 to complete your application. In addition, a USMLE Step 2 or COMLEX Step 2 score is preferred. For more information on our program, contact Kari Kazen, program coordinator.
All visiting medical student applications must be submitted through the Visiting Student Learning Opportunities program (formerly known as VSAS). For more information on visiting medical student opportunities, please visit our Visiting Learner page.
Salary and benefits
Corewell Health in West Michigan provides a comprehensive and very competitive benefits package for our residents, staff and their families. In addition, our program provides educational monies to support your ongoing education. Download our salary and benefits document to learn more.
Explore West Michigan

Program Director
Emergency Medicine
- Residency: Grand Rapids Education Partners/Michigan State University
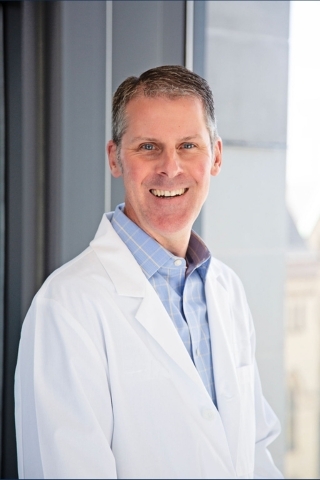
Emergency Medicine
- Residency: Grand Rapids Education Partners/Michigan State University
Associate Program Director
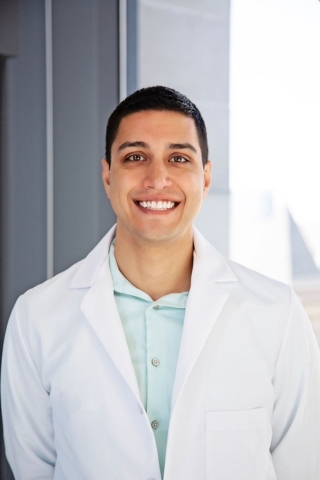
Emergency Medicine
- Residency: Grand Rapids Education Partners/Michigan State University
Emergency Medicine
- Residency: Grand Rapids Education Partners/Michigan State University
Core Faculty
Emergency Medicine
- Residency: St. Mary Mercy Hospital

Emergency Medicine
- Residency: Spectrum Health/Michigan State University
- Fellowship: (Emergency Ultrasound) Spectrum Health
Emergency Medicine
- Residency: Beaumont Hospital - Royal Oak

Emergency Medicine
- Residency: Spectrum Health/Michigan State University
Emergency Medicine
- Residency: St. Mary Mercy Hospital

Emergency Medicine
- Residency: Spectrum Health/Michigan State University
- Fellowship: (Emergency Ultrasound) Spectrum Health
Emergency Medicine
- Residency: Beaumont Hospital - Royal Oak

Emergency Medicine
- Residency: Spectrum Health/Michigan State University

Emergency Medicine
- Residency: University of Michigan Health System

Emergency Medicine
- Residency: Spectrum Health/Michigan State University
- Fellowship: Western Michigan University - Homer Stryker MD School of Medicine
Emergency Medicine
- Residency: Western Michigan University - Homer Stryker MD School of Medicine

Emergency Medicine
- Residency: Cleveland Clinic Foundation
- Fellowship: University of Michigan Health System
PGY 1

Ross University

Des Moines University

Ross University

Des Moines University
A.T. Still University—Kirksville College of Osteopathic Medicine

Central Michigan University

Kansas City University
Central Michigan University

Michigan State University
Western Michigan University
PGY 2

Chicago Medical School — Rosalind Franklin University

Wayne State University
Central Michigan University
Ross University

Chicago Medical School — Rosalind Franklin University

Wayne State University
Central Michigan University
Ross University
American University of the Caribbean

Kansas City University
Northwestern University

Michigan State University College of Human Medicine

Edward Via College of Osteopathic Medicine
University of Louisville
Michigan State University College of Osteopathic Medicine
PGY 3

St. George's University School of Medicine

University of Wisconsin School of Medicine and Public Health

Pacific Northwest University of Health Sciences College of Osteopathic Medicine

Michigan State University College of Osteopathic Medicine

St. George's University School of Medicine

University of Wisconsin School of Medicine and Public Health

Pacific Northwest University of Health Sciences College of Osteopathic Medicine

Michigan State University College of Osteopathic Medicine

Oklahoma State University Center for Health Sciences College of Osteopathic Medicine

Michigan State University College of Human Medicine

Des Moines University School of Medicine

Indiana University School of Medicine

Michigan State University School of Medicine

Marian University College of Osteopathic Medicine
Emergency medicine residency bios

Ready to Apply?
Review the “Application Requirements” tab on the program page to learn more about the application process.
