Epilepsy fellowship

The Corewell Health – Grand Rapids/Michigan State University Epilepsy Fellowship is a one-year, ACGME-accredited program that accepts two fellows per year. Clinical rotations take place at the Corewell Health in West Michigan Comprehensive Epilepsy Program, the largest and busiest Epilepsy Center in West Michigan and a NAEC Level 4 Epilepsy Center. The fellowship program provides a robust clinical and educational experience that encompasses all aspects of epilepsy care, with a special emphasis on epilepsy surgical management, neuromodulation and ICU-EEG monitoring.
Overview
The goal of our training program is to prepare individuals to be well-rounded, competent clinical epileptologists. This is accomplished through our educational program which is designed to provide increasing responsibility in patient care so that the fellow reaches a level of competence in the independent care of patients with epilepsy by the end of their training. It is our expectation that trainees provide excellent and compassionate care to patients with epilepsy, become life-long independent learners, and enhance their understanding of themselves and others in regards to epileptic disorders. In addition, fellows will function expertly in increasingly complex team-based patient care systems by the time they complete their training. All training is provided in an environment that maximizes fellow education, patient safety and the well-being of the fellows.
Program aims
By the completion of the training program, fellows will develop:
- Competence in the comprehensive diagnosis and management of all common and uncommon forms of epileptic disorders, including medical, surgical, emergent/critical care, and cognitive/behavioral/psychiatric aspects.
- Competence in the diagnosis and management of disorders that mimic epilepsy.
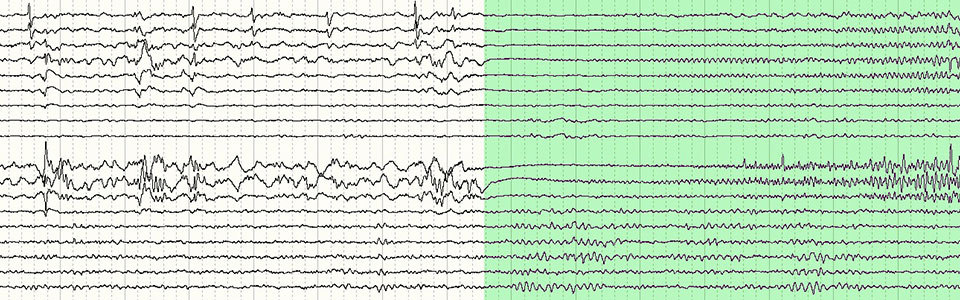
- Skill in interpretation of routine EEGs, as well as video-EEG monitoring, including scalp monitoring and intracranial monitoring.
- Skill in interpreting and performing tests/procedures essential to the diagnosis and management of pharmacoresistant epilepsy.
- Comprehensive knowledge of established and evolving biomedical, clinical, epidemiological and social-behavioral sciences, as well as the application of this knowledge to patient care.
- An understanding of the principles, indications, contraindications, risk, cost, and expected outcome of the various treatments and diagnostics.
- Competence in communicating diagnosis and treatment plans in a clear and compassionate manner to patients with varied backgrounds, educational experience and coping mechanisms. The ability to communicate professionally, accurately and clearly with other health care professionals, with a proper acknowledgement of the principles of HIPAA regulations.
- The ability to incorporate self-assessment and self-improvement practices in their plan as a life-long learner.
- The ability to apply practice and systems improvement, to allow an emphasis on patient safety and quality of care.
- Competence in evidence-based practice applied to clinical decision making.
- Knowledge of clinical trial design and statistical testing, as well as the ability to utilize this knowledge for critical interpretation of medical literature so as to become good consumers of new medical knowledge.
- Participation in the process of biomedical research through involvement in research projects.
- Competence in the education of other health care providers.
- Skill in working with, and leading patient care teams with a variety of providers and care givers to ensure an excellent level of patient safety and satisfaction.
Education
Rotations
Our academic year is divided into 13 blocks of four weeks each. Epilepsy fellows spend 11 blocks (44 weeks) at Corewell Health Butterworth Hospital (part of Corewell Health Grand Rapids Hospitals), and two blocks (eight weeks) at Corewell Health Helen DeVos Children's Hospital (part of Corewell Health Grand Rapids Hospitals).
- Butterworth Hospital has a nine-bed adult Epilepsy Monitoring Unit (EMU) and a busy epilepsy surgery program. This is the primary site for the epilepsy fellowship program. Butterworth Hospital offers a full spectrum of epilepsy care services for adults, including intracranial video-EEG monitoring, stereoelectroencephalography, electrocorticography, Wada testing, ICU-EEG monitoring and advanced neuroimaging. Outpatient epilepsy clinics and Neurostimulation Clinics with fellows will also take place at this site.
- Helen DeVos Children’s Hospital is a state-of-the-art children’s hospital with an excellent regional reputation for patient care. The hospital has a six-bed pediatric Epilepsy Monitoring Unit and an epilepsy surgery program. It is the site for pediatric rotations for the epilepsy fellowship program. Butterworth Hospital and Helen DeVos Children’s Hospital are busy neurodiagnostic centers, with more than 7,500 outpatient and inpatient (routine and continuous) EEGs completed annually.
Four non-consecutive blocks (16 weeks) of adult EEG training are planned for each fellow.
- All fellows are on a four week introductory EEG rotation for the first academic block of the year. During these weeks, fellows participate in a structured EEG didactics course covering basic and clinical EEG topics. They are provided education on EEG patterns associated with, and management of status epilepticus. During this block, fellows spend three days per week reading and reporting routine inpatient and outpatient EEGs. The emphasis during this block is normal EEG, common epileptiform and non-epileptiform abnormalities, artifacts, and normal EEG variants.
- During subsequent EEG blocks, fellows continue to advance their knowledge of routine outpatient and inpatient EEG. Butterworth Hospital has a busy continuous ICU and non-ICU video-EEG service, and fellows on their second, third, and fourth EEG blocks spend a majority of their rotation reading continuous video-EEG.
Six non-consecutive blocks of adult Epilepsy Monitoring Unit (EMU) experience are provided to each fellow.
- Fellows read and report video-EEGs on a wide variety of patients including diagnostic evaluations (such as patients being evaluated for seizure-like episodes and psychogenic non-epileptic seizures), Phase 1 (pre-surgical) evaluations, ictal SPECT evaluations, and Phase 2 evaluations (including subdural grids, depth electrodes, and stereoelectroencephalography). Our nine-bed adult EMU admits, on average, two to three Phase 1 patients per week, two ictal SPECT patients per week, and two to four Phase 2 patients per month. This ensures a robust clinical-educational experience for fellows. Patient volume and complexity will be variable, based on fellow experience. In addition, daily EEG teaching rounds occur.
- Mid-fellowship and advanced level fellows on the EMU rotations also participate in cortical stimulation, Wada testing, and intra-operative electrocorticographic recordings. The fellows’ clinical experience in the EMU involves direct patient management.
- On the primary EMU service, fellows admit patients, round on admitted patients, and discharge patients. Fellows also complete an inpatient consultation and provide recommendations on EMU patients undergoing video-EEG monitoring and not admitted to the primary EMU service. Additional inpatient consultations are completed on ICU and non-ICU patients with seizure disorders, as requested by the inpatient neurology teams.
Each epilepsy fellow spends two blocks on pediatric epilepsy rotations at Helen DeVos Children’s Hospital.
- A total of two to three weeks during the two blocks are dedicated to reading and reporting pediatric and neonatal routine EEGs.
- Two weeks during these blocks are dedicated to reading and reporting pediatric and neonatal continuous ICU video-EEGs.
- Two to three weeks during the two blocks are dedicated to reading and reporting pediatric video-EEGs performed in the six-bed pediatric EMU at Helen DeVos Children’s Hospital; these include Phase 1 and Phase 2 studies.
- Fellows attend one half day of pediatric epilepsy clinic per week and actively participate in the pediatric epilepsy surgery case discussions.
Epilepsy fellows on EEG, EMU and pediatric epilepsy rotations have overnight home-call responsibilities. There is no in-house overnight call. Additionally, fellows have weekend rounding and EEG interpretation assignments for two weekends each block; all fellows have two weekends (four days) per block free of all educational and clinical responsibilities.
The epilepsy clinic at Corewell Health Butterworth Hospital (part of Corewell Health Grand Rapids Hospitals) has 18 clinic examination rooms.
- Each fellow is assigned two half days of epilepsy clinic per week at this suite throughout their fellowship year, one of these Clinics is the Fellows' own continuity clinic experience. Fellows evaluate all new and returning adult epilepsy patients in the clinic under faculty supervision.
- The epilepsy fellow on EMU rotation attends two half days of Neuromodulation Clinic per EMU block at this site; this furthers the fellows’ experience with approved devices for epilepsy.
Each fellow is provided one block of elective time. A variety of elective options are available (such as critical care EEG monitoring, neuropsychology and psychotherapy, neuromodulation, neuroradiology, research). Fellows may elect to spend all elective block time in one area or split time between two areas (two weeks each). Fellows have no call commitments while on elective but continue to participate in epilepsy clinics.
Didactics
A variety of seminars and conferences are planned to further fellow education. Fellows attend dedicated epilepsy and EEG didactic lecture series throughout their fellowship year covering all basic science and clinical aspects. Fellows also participate in our weekly multidisciplinary epilepsy surgical conference. Additionally, epilepsy guest lectures, journal clubs, and EEG case conferences are offered, each of these conferences occurs monthly.
Fellows attend neurosciences grand rounds and are invited to present once at Grand Rounds in the last three months of their fellowship year. A morbidity, mortality and practice improvement conference is also offered monthly.
Research and teaching opportunities
All fellows participate in a didactic program to become familiar with the methods, regulations and ethics involved in the conduct of responsible research. The fellowship program mandates participation in an eight lecture series in the early part of the fellowship that provides the fellow with training and experience in planning and conducting research, and education on how to be better consumers of clinical research. This series furthers fellows' knowledge of the ethical considerations involved in clinical research, hypothesis generation and data analysis, mastering skills for scientific writing, and making oral presentations. The topics covered also help fellows understand concepts of evidence-based medicine and putting those into practice.
The Corewell Health Research Institute provides resources, support for research, and oversight of research facilities. This office of research has established an IRB and manages research grants and contracts. It supports a broad range of research including clinical trials, translational research, and basic science research. In addition, the Corewell Health Office of Medical Education in West Michigan has a scholarly activity support division that assists residents and fellows with research projects, including educating residents and fellows about research regulations, IRB submission, data analysis, and publication. Michigan State University College of Human Medicine has also recently expanded their research facility and resources are available to residents and fellows through this entity. The epilepsy fellowship faculty has a wide variety of clinical interests and is available to mentor fellows participating in scholarly activity. Fellows are expected to participate in ongoing departmental research projects or lead their own projects, and are expected to take projects to completion through publication, or presentation as an abstract at a local, regional, national or international level meeting. Epilepsy fellows receive support to attend at least one regional, national, or international professional conference during their training program.
Epilepsy fellows have several opportunities to further their teaching skills. In addition to the expected presentations at multidisciplinary epilepsy surgical conferences, EEG case conferences, and journal clubs, during the second half of their fellowship year epilepsy fellows are expected to lead (a) two neurology residency didactic lectures in epilepsy, (b) two didactic sessions for EEG technicians, (c) two educational offerings for nursing/clinic staff, and (d) two epilepsy patient support group meetings. This ensures educational skills are developed to cater to a variety of audiences.
Application requirements
We recruit for two positions each year at the PGY-5 level. Eligibility requirements include:
- Applicants must complete a four year ACGME-accredited Neurology residency program before entry into the fellowship program. Applicants who complete an RCPSC-accredited or CFPC-accredited residency program located in Canada before entry into the fellowship program are also eligible
- Applicants must possess U.S. work authorization or be eligible for J-1 visa status
- Applicants must be a MD/DO or equally acceptable degree
- Applicants must have strong communication skills
- We do not have minimum USMLE Step 1, Step 2 CK or Step 3 Score requirements.
Effective with the 2024-2025 academic year, we will be participating in the National Residency Matching Program (NRMP). Applications will only be accepted through the Electronic Residency Application Service (ERAS). Three letters of recommendation are required; One letter of recommendation must be from the neurology residency program director where you most recently trained.
Completed applications are reviewed by the epilepsy fellowship program director and an invitation to interview will be extended to qualified applicants. Invited applicants are interviewed by the program director and epilepsy faculty. Interviewers rate each applicant independently and decisions regarding appointments to the fellowship are made by consensus.
If you have any questions, require more information on our program or wish to inquire about available positions, please contact us at EpilepsyFellowship@spectrumhealth.org
Explore West Michigan
Program Director
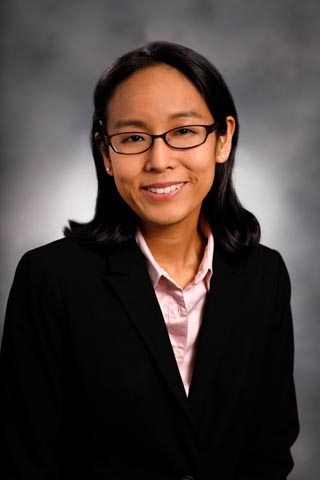
Epileptologist
Specialty: Epilepsy
- Fellowship: Mayo School of Graduate Medical Education
- Residency: Mayo School of Graduate Medical Education
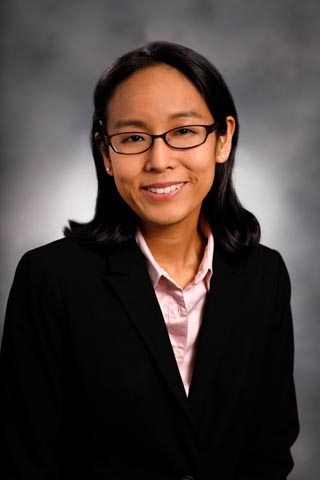
Epileptologist
Specialty: Epilepsy
- Fellowship: Mayo School of Graduate Medical Education
- Residency: Mayo School of Graduate Medical Education
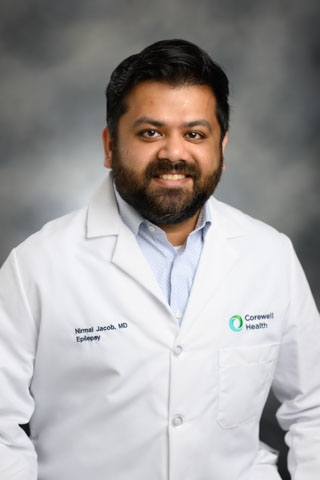
Core Faculty

Epileptologist
Specialty: Epilepsy
- Fellowship: University of Michigan
- Residency: Garden City Hospital

Epileptologist
Specialty: Epilepsy
- Fellowship: University of Michigan Health System
- Residency: Boston University Affiliated Hospitals

Epileptologist
Specialty: Epilepsy
- Residency: St. Joseph’s Hospital

Epileptologist
Specialty: Pediatric Neurology, Epilepsy
- Fellowship: University of Michigan Health System
- Residency: Nationwide Children’s Hospital & Ohio State University

Epileptologist
Specialty: Epilepsy
- Fellowship: University of Michigan
- Residency: Garden City Hospital

Epileptologist
Specialty: Epilepsy
- Fellowship: University of Michigan Health System
- Residency: Boston University Affiliated Hospitals

Epileptologist
Specialty: Epilepsy
- Residency: St. Joseph’s Hospital

Epileptologist
Specialty: Pediatric Neurology, Epilepsy
- Fellowship: University of Michigan Health System
- Residency: Nationwide Children’s Hospital & Ohio State University

Epileptologist
Specialty: Epilepsy
- Fellowship: Mayo Clinic
- Residency: Mayo Clinic

Epileptologist
Specialty: Pediatric Epilepsy
- Fellowship:
- (Child Neurology)University of Pittsburgh Medical Center, Children’s Hospital of Pittsburgh
- (Pediatric Epilepsy, Clinical Neurophysiology) University of Pittsburgh Medical Center, Children’s Hospital of Pittsburgh
- Residency: Michigan State University – Kalamazoo Center for Medical Studies

Epileptologist
Specialty: Epilepsy
- Fellowship: University of Minnesota
- Residency: University of Minnesota

Epileptologist
Specialty: Epilepsy
- Fellowship: University of Michigan Health System
- Residency: Michigan State University Statewide Campus System Garden City
PGY 5
Neurology: Sparrow Hospital/Michigan State University
Neurology: Sparrow Hospital/Michigan State University
Ready to Apply?
We participate in the National Resident Matching Program and use the Electronic Residency Application Service.
